Members:
Angela Mehta
Naomi Moehn-Aguayo
Tyler Paik
Summary:
Diabetes is a chronic disease were the effected person is unable to properly produce or utilize insulin, a hormone produced by the pancreas (WHO Writers, Unknown). As a result, a diabetic person is unable to regulate their own blood-sugar levels, which can lead to serious health complications with time, including heart disease, vision loss, nerve damage, and kidney disease. Treatment depends on the type of diabetes and ranges anywhere from oral medication to relying on a mechanical pump to continuously inject insulin into the afflicted person (WHO Writers, Unknown).
The "Diabetes 130-US Hospitals for Years 1999-2008" is an extensive dataset of over 100,000 entries, measuring the clinical care of patients with diabetes collected over the course of ten years. The main focus of the dataset was to observe whether or not diabetic patients were readmitted to hospitals within 30 days of being discharged and what factors may have led to them coming back (Strack et. al., 2014). The study itself was conducted because, despite evidence showing that the quality of treatment towards diabetic patients has greatly improved, many patients still fail to receive adequate care. Lack of proper treatment may seriously impact patient mortality and morbidity, and lead to further complications associated with diabetes. The study partially attributes this negligence to "arbitrary diabetes management" in some hospital environments (Strack et. al., 2014).
In order to properly analyze the data given our limited timeframe, our group only worked with a small portion of this dataset, focusing on patients who ranged from 30 to 50 years of age. We used the data to deduce whether diabetic patients were receiving inadequate treatment during their visits, and if so how exactly they were neglected. In doing so we hope to better understand how diabetic patients experience discrimination in the healthcare industry and what steps could be taken to better treatment in the future. We primarily used Poirier's denotative reading in our analysis of the data because, by looking at the data with an objective lens, we could better understand why researchers chose to look into the factors they did. With this perspective, along with a few points from utilizing Koopman’s Sociological Format Anatomies of Experience and Use, we could figure out specific points of interest that may be tied to negligence and/or discrimination.
Conclusion:
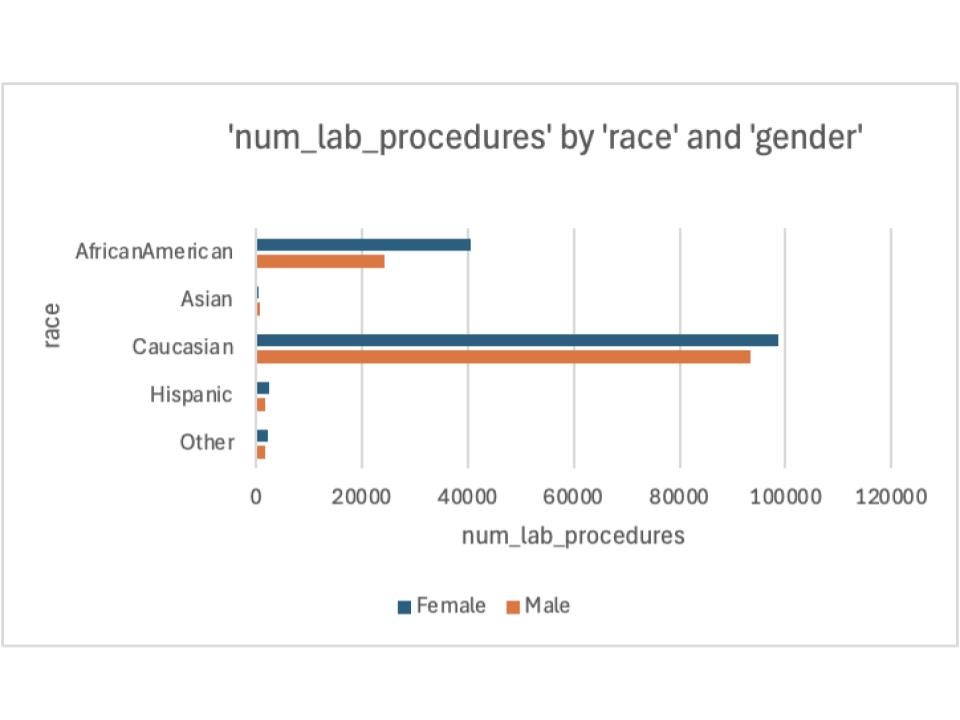
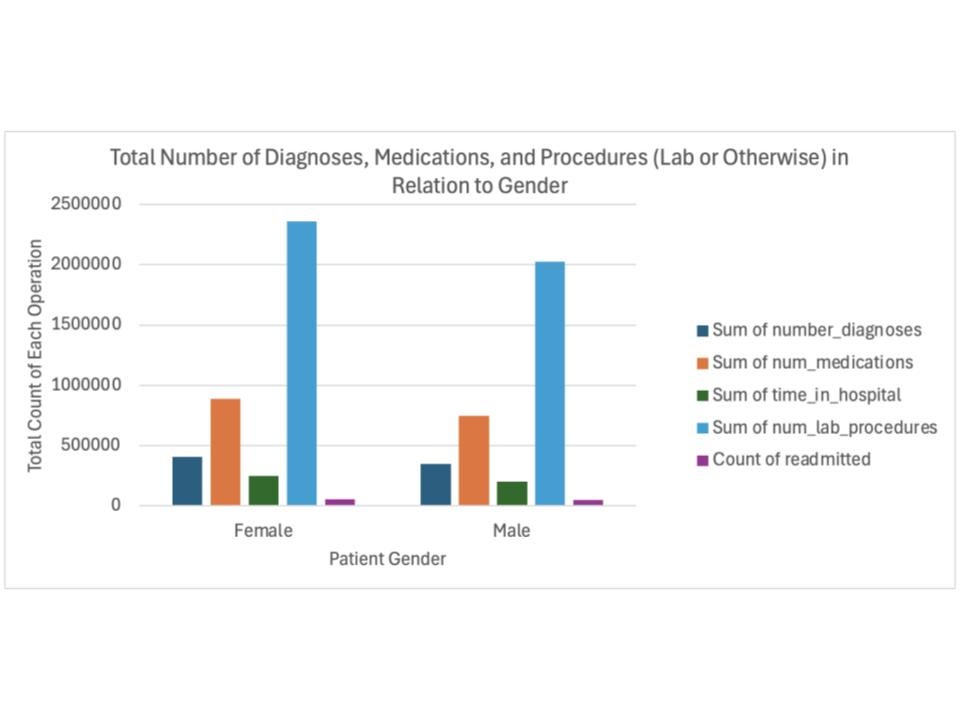
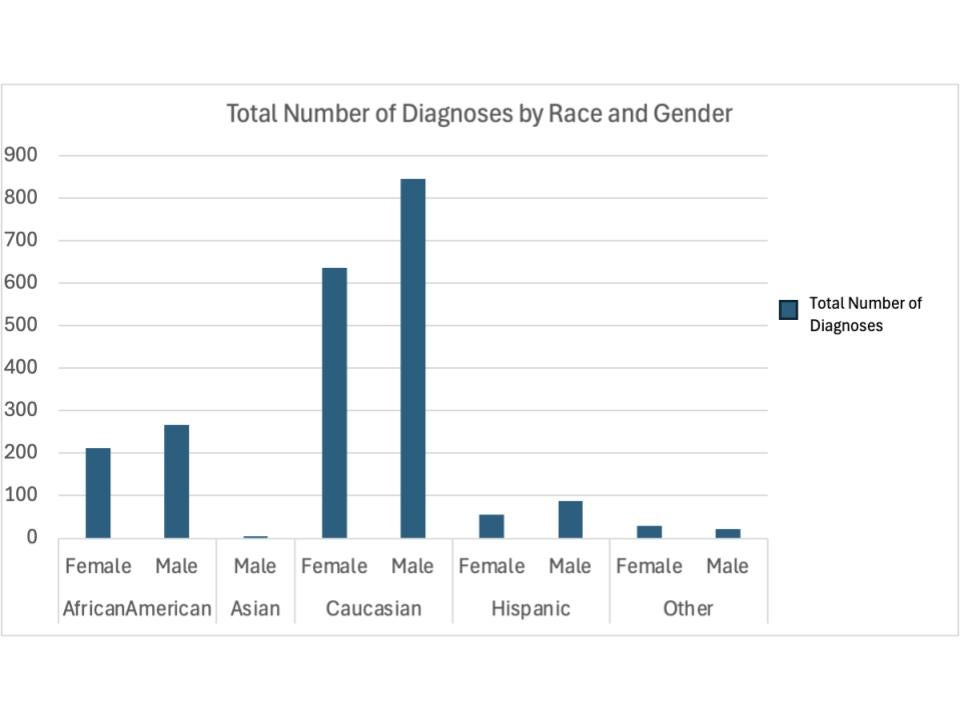
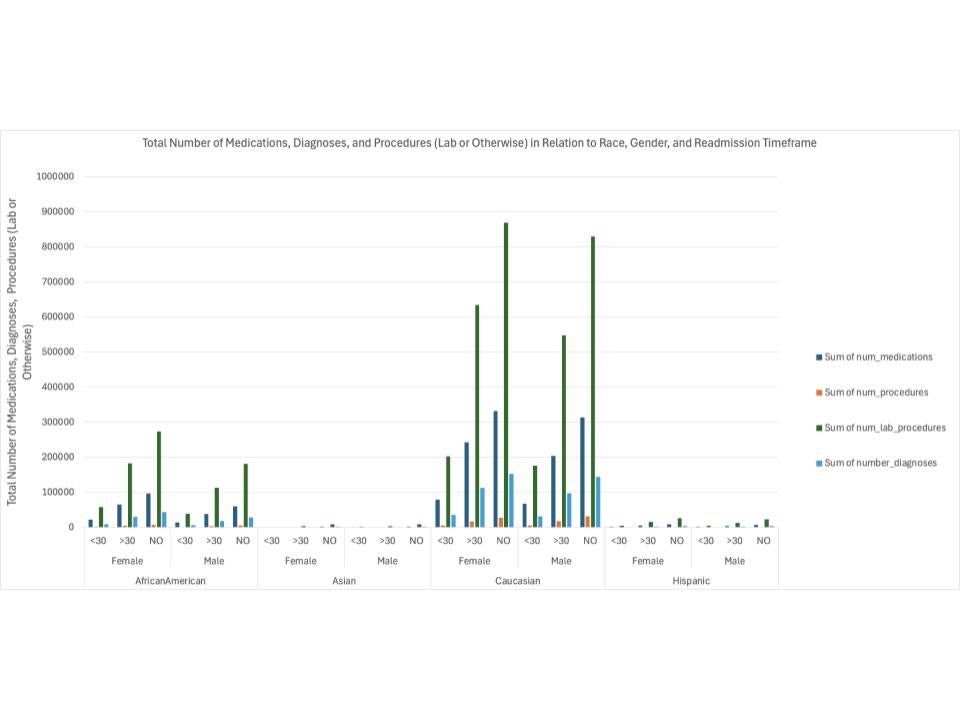
Based off of the data and looking at a multitude of factors (like race, gender, # of diagnoses, etc.), our group found that caucasian women within the 30-50 age range received the most treatment (i.e. diagnoses, tests, medication, etc.), followed by African Americans, Hispanics, then Asians, respectively. Caucasian women also were least likely to be readmitted within 30 days of their initial discharge, with the same trend regarding race continuing. It is important to note however, we only had one case of an Asian patient, following a trend of very limited data surrounding Asian diabetic patients within this study (642/101,767 or ~0.631% of the entire dataset). This could potentially be attributed to the fact that the hospitals used for this study were all relatively small and primarily located in the Northeast of the US (58/130) (Strack et. al., 2014).
Our group used the "Diabetes 130-US Hospitals for Years 1999-2008" dataset to determine whether or not diabetic patients were being neglected during their hospital.